How Cardiology Providers Can Improve Outcomes Without Increasing Clinical Burden?
Improving cardiology outcomes is now vital as healthcare moves to value-based models. However, the traditional approach creates a risky paradox. Cardiology teams are seeing more complex patients and more quality metrics, while also working at full capacity, amplifying clinical burden in healthcare at every step of cardiology care delivery.
Nearly 43% of cardiologists report burnout, with 68% citing bureaucratic tasks as the primary cause. Cardiology nurses face 59% burnout rates, the highest among cardiovascular staff. Sustainable improvement in cardiology care delivery cannot depend on heroic individual effort. Successful programs boost cardiology outcomes with smarter systems.
Why Clinical Burden Is a Growing Problem in Cardiology?
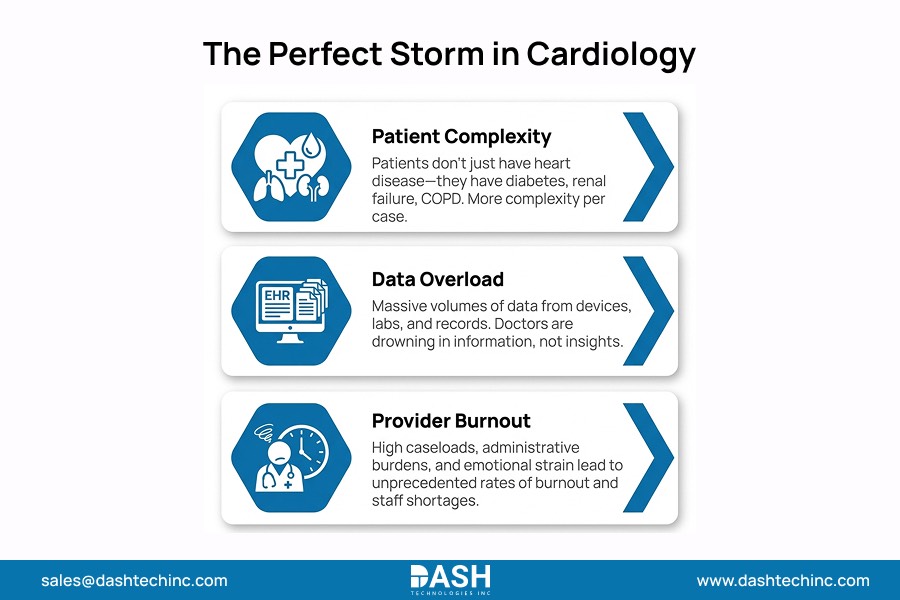
The “perfect storm” of factors is making cardiology one of the most high-pressure specialties in medicine. Cardiology clinician burnout is at an all-time high. This rise mainly comes from factors outside direct patient care.
Increasing Patient Complexity
The average patient that a cardiologist sees these days doesn’t just have heart disease. They typically have diabetes, renal failure, chronic lung disease, etc. That means more complexity in managing their primary cardiac issue.
Documentation and Reporting Demands
The cardiology documentation burden has exploded. Clinicians often spend more time clicking through EHR screens for regulatory compliance. This takes away from the time they could spend discussing treatment plans with patients.
Fragmented Clinical Workflows
Cardiology care is naturally spread out across different settings. It takes place in the inpatient ward, the cath! lab, outpatient clinics, and through remote monitoring. When these systems don’t communicate, clinicians must “connect the dots.” This adds to the exacerbating healthcare workforce challenges.
Why Traditional Outcome Improvement Efforts Often Backfire?
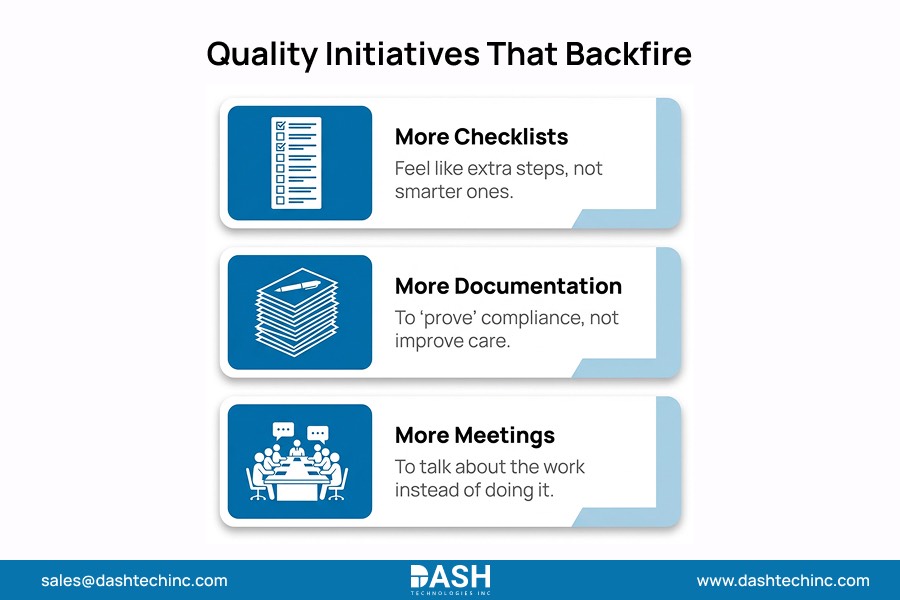
Outcome improvement healthcare efforts can fail when they treat clinicians as the “engine” of change rather than designing the system to make the right action the easy action. Many cardiology quality initiatives start with good intentions, but add layers of work.
Common patterns that backfire:
- More checklists that feel like extra steps, not smarter steps
- More documentation to “prove” compliance rather than improve care
- More manual tracking in spreadsheets, emails, or ad hoc reports
The result is clear. Outcomes may improve for a time as the project team works hard. However, the cardiology clinical burden will increase permanently. Over time, clinicians disengage, variation returns, and burnout rises.
The Shift Toward System-Level Outcome Improvement
A system-level healthcare improvement strategy assumes that clinicians are already doing their best. Instead of asking them to work harder, it focuses on cardiology care optimization by fixing the environment they work in.
A practical definition: System-level improvement refers to the redesign of organizational processes, data flows, and technological infrastructures to achieve better results automatically, reducing the reliance on human memory or manual intervention.
By focusing on the system, leadership ensures that the “right way” to provide care is also the “easiest way.”
How Data and Analytics Improve Cardiology Outcomes Behind the Scenes?
This is where cardiology analytics acts as a silent partner for improving cardiology outcomes. Instead of adding a task to a doctor’s plate, data-driven cardiology works in the background to surface insights.
Identifying Variation in Care and Outcomes
Clinical performance analytics can highlight where one facility or provider has significantly different outcomes than others, allowing for targeted training without broad, department-wide mandates.
Supporting Earlier Intervention
Risk models and rules-based monitoring can identify patients trending toward decompensation, nonadherence, or missed follow-ups. The goal is not to generate more alerts; it’s to route a small number of high-confidence actions to care teams (e.g., “needs outreach in 48 hours”).
Proactive Rather Than Reactive
Analytics supports proactive care by highlighting leading indicators, such as:
- Missed follow-up after ED visit for chest pain or HF symptoms
- Rising weight/BP trends from remote monitoring (when available)
- Delayed post-procedure check or anticoagulation monitoring gaps
When designed well, clinicians receive curated insights, not additional documentation or manual reviews.
Read More




Comments
Post a Comment