How Leading Orthopedic Providers Leverage Analytics to Optimize OR Utilization and Margins?
Orthopedic operating room utilization is no longer just an operations metric. It’s a key component of orthopedic service line performance success and driving hospital margins orthopedics. Top performing providers are leveraging orthopedic OR utilization analytics to enhance their OR data and drive improvements to OR efficiency, patient care, and hospital OR performance. OR throughput fuels the revenue engine of your orthopedic program. Small inefficiencies become millions of dollars in margin losses when multiplied by joint replacements and spine cases.
OR utilization is no longer just a performance metric — but understanding why orthopedic departments struggle to turn surgical data into actionable insights is the first step toward improvement.
Why OR Utilization Is a Critical Challenge for Orthopedic Departments?
Orthopedics presents a uniquely complex operating room environment and OR utilization challenges. High demand and high variability collide, making traditional planning approaches inadequate, exposing orthopedic OR inefficiencies.
- High Case Volume, High Variability
Orthopedic cases come in high volume, often several hundred per day. But case length, required equipment, staffing needs, and complexity can vary widely from case to case. - Surgeon Preference and Scheduling Complexity
Surgeons often have distinct preferences for implants, teams, and workflows. Aligning block time, staff, and equipment for multiple surgeons causes scheduling issues. This leads to delays in surgical throughput. - Rising Costs and Margin Pressure
From labor shortages to implant costs to reimbursement changes, margins are under pressure. Running efficiently isn’t optional; it’s a requirement to maintain your budget.
Manual OR planning cannot keep up with this complexity. Analytics enables leaders to see patterns across surgeons, procedures, and facilities that manual processes miss
What Poor OR Utilization Looks Like in Orthopedic Programs?
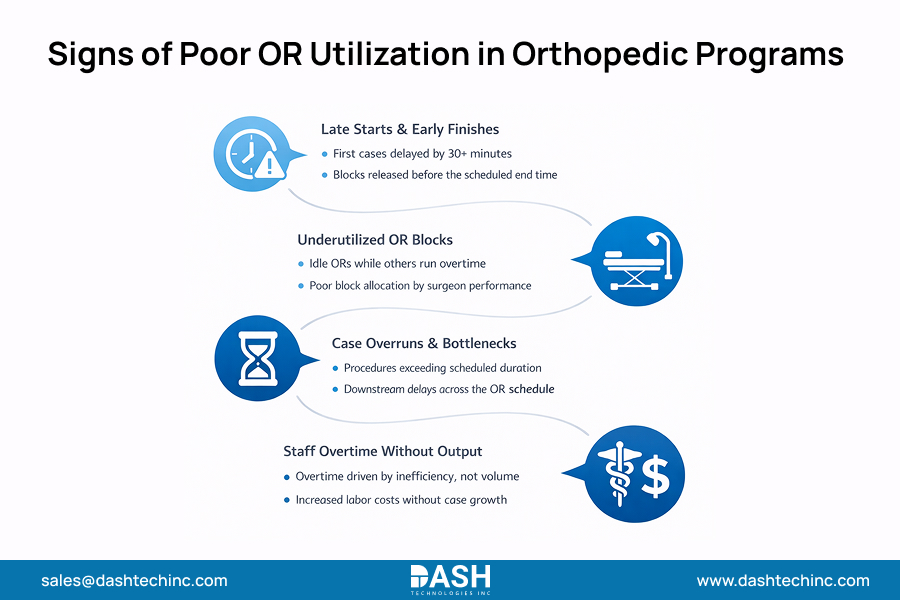
Poor OR block utilization manifests in recognizable patterns that drain margins and frustrate staff:
- Late starts and early finishes – First cases beginning 30+ minutes late and surgeons releasing blocks hours early
- Underused OR blocks – Allocated time sitting empty while other ORs run over capacity
- Case overruns and bottlenecks – Procedures consistently exceeding scheduled time, creating domino delays
- Staff overtime without productivity gains – Teams working extra hours not because of high volume, but poor scheduling
Delays in scheduling push cases to later dates. This raises costs and also lowers patient satisfaction. These are symptoms of underlying problems, not random events. Without analytics, leadership teams may struggle to distinguish patterns from noise.
Why Traditional OR Reports Fail to Drive Improvement
Most orthopedic leaders are drowning in data but starving for orthopedic OR utilization analytics. Traditional orthopedic performance reporting typically relies on retrospective healthcare reporting, static spreadsheets that arrive weeks after the month has ended.
The primary OR reporting limitations include:
- Lagging Indicators: Realizing you had poor utilization last month doesn’t help you improve tomorrow’s schedule.
- Lack of Granularity: Without being able to drill reports down by surgeon/procedure type/facility/etc. You won’t know where delays are actually occurring.
- Data Silos: When scheduling data, EHR data, and financial data live in different systems, the “full picture” of an orthopedic program remains invisible.
To truly grasp why traditional orthopedic performance reporting falls short, revisit these common orthopedic performance reporting challenges.
How Analytics Changes the Way Orthopedic Leaders Manage ORs?
Modern operating room analytics in healthcare move the needle by shifting the focus from “what happened” to “why it happened and how to fix it.”
- From Historical Reports to Real-Time Visibility
Orthopedic analytics platforms provide live dashboards that allow clinical managers to see exactly where a case stands. This real-time visibility enables “active management”—adjusting the next case’s start time or reassigning staff before a delay becomes a crisis. - Standardizing OR Performance Metrics
Instead of leadership hearing anecdotal comments (“The OR always runs slow”) the facts are based on real-time OR insights. Standardize metrics across the service line so everyone measures performance the same way, creating a culture of accountability. - Turning Variability Into Predictable Patterns
Analyzing thousands of past cases, analytics can predict actual case durations much more accurately than a surgeon’s estimate. This cuts down on “buffer time” and leads to a tighter, more efficient schedule. - Read More




Comments
Post a Comment