Intelligent Orthopedic Care: How AI & Data Revolutionize Arthroplasty Outcomes
Orthopedic surgery is not what we knew it used to be. Hospitals and surgeons are now expected to deliver precise, predictable, and patient-specific joint replacement outcomes. This is in addition to their increasing caseloads, complex patient profiles, and operational challenges.
This is where intelligent orthopedic solutions based on AI in orthopedic surgery are revolutionizing the treatment of orthopedic patients. Right from pre-op planning to conducting the surgery and post-op recovery, data-driven orthopedic care is ensuring that orthopedic patients are treated not through intuition but through standardized treatment processes.
Imagine a hospital preparing for a knee replacement. AI-powered orthopedic systems examine the patient’s scans, indicate possible complications, and recommend the best possible positions for the implant. During surgery, intelligent guidance ensures accurate implantations during the surgery. After discharge, the wearable sensors allow for constant patient surveillance and early intervention.
Hospitals and MedTech teams adopting AI-enabled orthopedic platforms aren’t experimenting anymore; they’re standardizing outcomes, improving efficiency, and scaling quality. But how does this look like inside real orthopedic workflows?
Let’s walk through it.
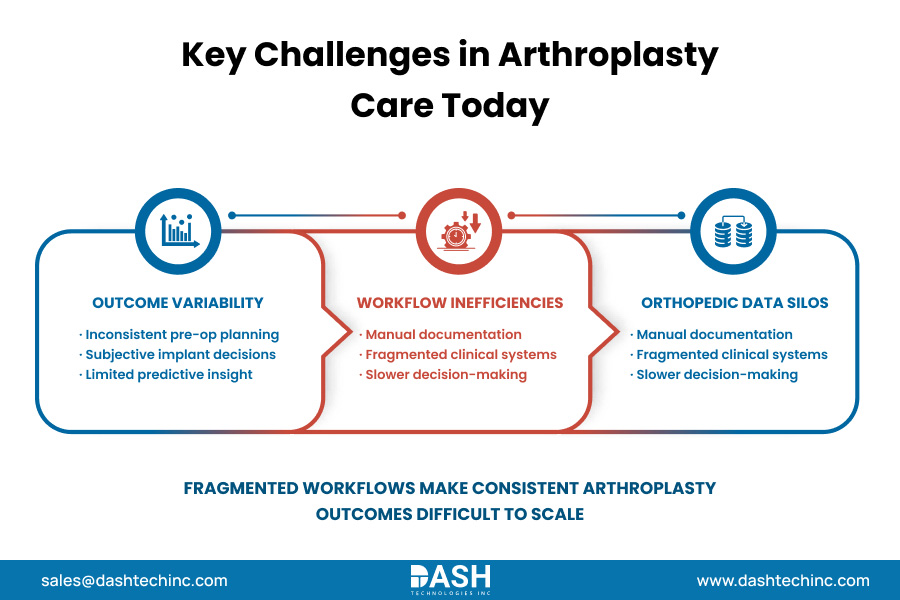
Top Challenges in Arthroplasty
Even with modern techniques, hospitals experience challenges in orthopedic surgery workflows, especially in arthroplasty units.
- Outcome variability remains high
Despite surgeon expertise, orthopedic surgery outcome variability persists due to inconsistent pre-op planning, implant selection, and execution. Reliance on 2D imaging and experience alone introduces avoidable risk. - Arthroplasty care inefficiencies slow teams down
Manual documentation, fragmented imaging systems, and disconnected tools contribute to inefficiencies in joint replacement surgery. These orthopedic clinical workflow challenges increase cognitive load and delay decisions. - Orthopedic data silos limit insight
Clinical, imaging, and registry data often live in separate systems, creating orthopedic data silos. This fragmentation makes real-time, evidence-based decisions difficult particularly at a large scale.
These challenges make one thing clear: it is no longer a choice whether to use integrated AI workflows—it is a necessity for reliable outcomes in arthroplasty.
What Makes Orthopedics “Intelligent”?
So, what does intelligent orthopedic care actually mean in practice?
It’s the convergence of intelligent orthopedic technology, connected systems, and workflow-aware AI:
- AI and robotics in orthopedics enable precision and repeatability in the OR
- Smart orthopedic care systems support decision-making across the care continuum
- Digital transformation in orthopedics enables a single workflow that links planning, surgery, and recovery.
Behind this capability is a connected ecosystem that supports consistent execution, not isolated innovation.




Comments
Post a Comment