Orthopedic Data Analytics: Turning Surgical Data into Better Outcomes and Smarter Decisions
Orthopedic teams have plenty of data available to them. What they really lack is clarity.
Most orthopedic departments and practices all over the U. S. are currently performing more procedures than ever before joint replacements, sports injuries, spine cases while at the same time, they have to deal with tighter margins, staffing…
Everyone agrees that data should be helpful. Actually, it often causes delays.
Spreadsheets arrive weeks late. Reports answered yesterday’s questions. Dashboards look impressive but don’t reflect how orthopedic care actually works.
That gap—between having data and using it confidently—is exactly where orthopedic data analytics proves its value.
The Real Problem Isn’t Data. It’s Fragmentation.
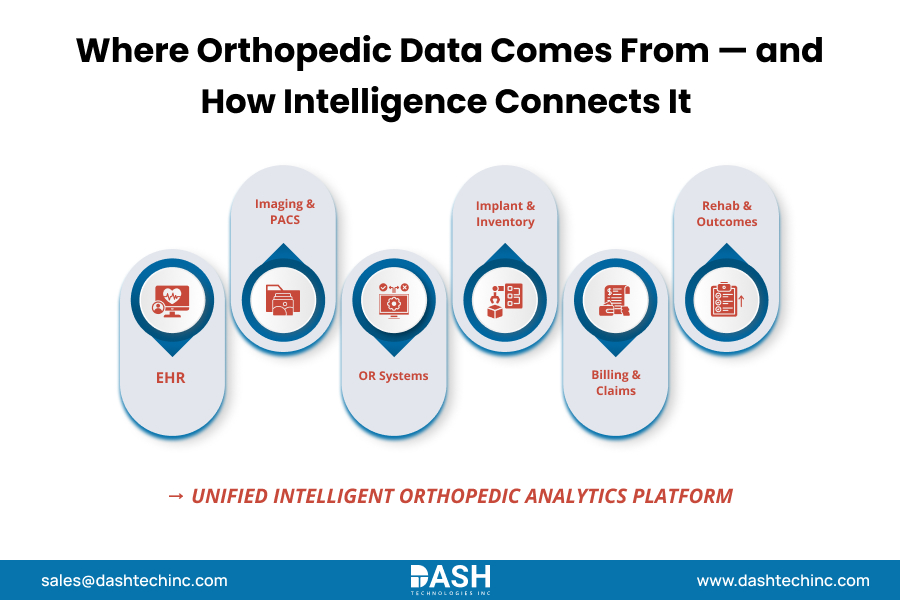
Orthopedics touches more systems than most service lines. Clinical notes live in the EHR. Images sitting in PACS. OR data comes from scheduling systems. Implant costs live somewhere else entirely. Billing and claims data arrive after the fact.
Each system works fine on its own. Together, they rarely tell a complete story.
For leadership teams, this creates real friction:
- Surgeons don’t trust reports that lack clinical nuance
- Administrators struggle to compare performance across sites or providers
- Finance teams see rising implant costs but can’t explain the variation
Without connected analytics, decisions rely on experience and intuition—valuable, but no longer sufficient in today’s environment.
What Orthopedic Data Analytics Actually Changes
When analytics are designed specifically for orthopedic workflows, they stop being “reports” and start becoming decision tools. The impact shows up in a few key areas.
Clearer Visibility into Surgical Outcomes
Instead of looking back at the results months later through a review, teams are now able to keep up with trends on different types of procedures, patient cohorts, or surgeons. It becomes quite easy to identify the patterns concerning the complications, the readmissions, and the recovery timelines at an early stage. There is still enough time to act if necessary.
More Predictable Length of Stay
Variation in LOS often has little to do with the procedure itself and everything to do with the process. Analytics helps identify where delays happen, whether it’s pre-op prep, post-op mobility, or discharge coordination.
Even small reductions add up quickly at scale.
Implant Cost Control Without Oversimplification
Implant spend is a sensitive topic. Surgeons want a choice. Finance wants consistency. Analytics bridges that gap by showing cost in context—paired with outcomes, not just price tags.
This supports informed discussions instead of blanket standardization.
Proactive Risk Identification
By means of predictive analytics, teams are enabled to identify higher, risk patients at an earlier stage. This leads to well, thought, out care, more focused patient education, and lesser post, surgery surprises.
It’s not about replacing clinical judgments. It’s about supporting it.
Smarter Use of OR Time and Staff
When OR utilization data is tied to real workflows, inefficiencies stand out. Block time, staffing, and turnover issues become easier to address—especially important for ASCs and high-volume programs.
Why Many Analytics Efforts Stall
Most orthopedic organizations already have analytics tools. What they lack is relevance.
Generic dashboards don’t reflect surgical pathways. Static reports don’t keep pace with operational reality. And when clinicians don’t trust the data, adoption stalls.
Effective orthopedic analytics works because it:
- Mirrors how orthopedic teams actually practice
- Connects clinical, operational, and financial views
- Delivers insight fast enough to matter
When that happens, conversations change. Decisions move faster. Alignment improves.




Comments
Post a Comment