Why Orthopedic Departments Struggle to Turn Surgical Data into Actionable Insights
Orthopedic departments hold more surgical data than any other service line. But many find it hard to gain useful insights from this information. Orthopedic data analytics challenges often arise not from too little information. Instead, they come from healthcare data fragmentation within orthopedic departments. Operating room logs, implant registries, imaging archives, patient reported outcome databases, the list of orthopaedic surgery related data captured in hospitals is staggering.
Orthopedic services create massive amounts of data each day. Still, leaders face one inescapable truth. They lack access to usable, timely intelligence. This data is crucial for choices that impact patient care, improve operational efficiency, and financial performance.
The data paradox isn’t caused by the shortage of data; healthcare data fragmentation is the reason orthopedic departments can’t solve their biggest challenges. When data is trapped in silos, it’s difficult, if not impossible, to connect the dots across systems. Service line directors, surgeons, and administrators don’t have real-time answers. Instead, they depend on old reports, incomplete data, or gut feelings. This lack of real-time evidence limits their decision-making.
The Volume and Complexity of Orthopedic Surgical Data
Orthopedic surgical workflows are complex & Orthopedic data analytics challenges are unique. This makes them different from most other areas in healthcare. Each step in the patient’s journey creates touchpoints across the entire continuum of care. These touchpoints generate distinct information streams. Over time, all these streams must converge to provide a complete clinical picture.
Orthopedic clinical data & orthopedic operational data sources include:
- Pre-operative assessments, patient histories, and diagnostic imaging
- Intra-operative documentation including surgical technique, implant selection, and procedural times
- Post-operative recovery metrics, rehabilitation progress, and long-term outcomes
- Imaging data from PACS (Picture Archiving and Communication System)
- EHR documentation spanning multiple care episodes
- Vendor-specific implant tracking systems and registries
- OR management platforms tracking utilization and turnover times
In many other service lines, a procedure is a singular event. In orthopedics, a procedure includes several factors: a specific surgeon, a certain vendor’s device, a patient’s BMI, and a rehab plan for follow-up. Each element plays a crucial role in the outcome. This collection of data points along the care continuum generates a lot of orthopedic surgical data. But without the right analytics tools, it’s hard to understand that data consistently. It also makes comparisons across locations or time tricky.
Fragmented Systems Create Data Silos Across Orthopedic Programs
The biggest barrier to orthopedic analytics is orthopedic data silos. Hospitals have used top systems for imaging, documentation, OR management, and supply chain operations. While effective individually, these systems were never designed to function as a cohesive ecosystem.
Disconnected Clinical and Operational Systems
Clinical documentation and operational execution often live in separate digital worlds. A surgeon documents the medical necessity for a total joint replacement in the EHR, while the implant for that procedure is managed in a standalone ERP system. In many cases, there is no automated link between the two.
This creates the “swivel chair” problem: This fragmented healthcare data forces the staff to move between systems to piece together performance insights. Without orthopedic system integration, calculating true cost-per-case becomes a manual exercise built on spreadsheets and assumptions, undermining confidence in the results.
Limited Interoperability Between OR, EHR, and Imaging
The lack of orthopedic system integration between critical platforms creates visibility gaps that impact both clinical and operational performance. When OR scheduling systems don’t share data with EHRs, and imaging archives remain disconnected from surgical documentation, leaders lose the ability to correlate inputs with outcomes.
Surgeons can’t easily compare their implant choices with recovery trajectories, and administrators struggle to identify which procedures deliver the best value. For departments seeking integrated solutions, platforms that enable comprehensive orthopedic data integration become essential to breaking down these barriers.
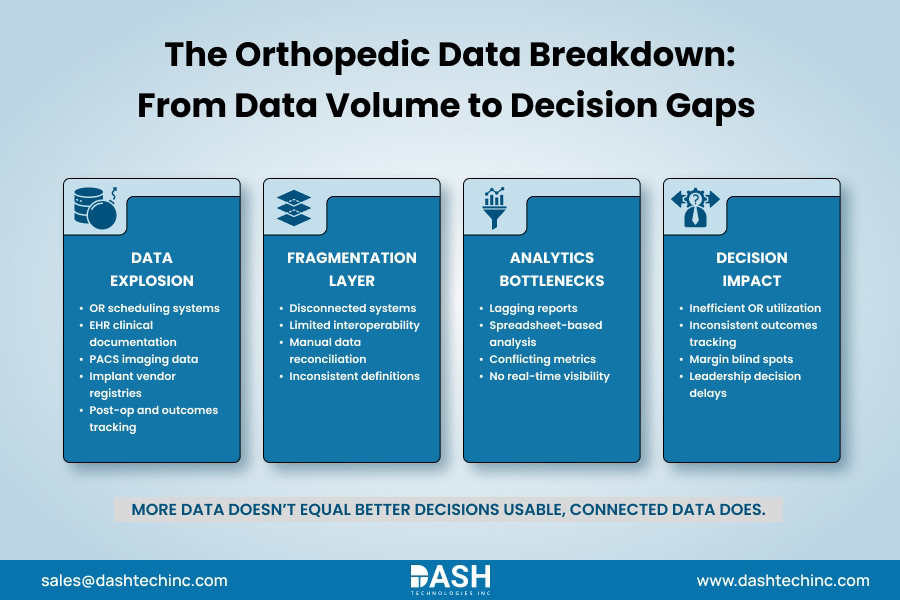
Why Orthopedic Data Rarely Translates Into Decision-Ready Insights
Even when hospitals successfully aggregate their data into a warehouse, the orthopedic analytics challenges don’t disappear; orthopedic data analytics challenges just shift. The raw material exists, but transforming it into actionable orthopedic insights is a different problem entirely.
Healthcare data usability suffers due to three main factors:
Raw Data ≠ Insight: 5,000 lines of surgical logs do not equal insight; it just means a big list. Without cleaning & standardization, raw healthcare data causes more problems than it solves. For example, if one surgeon documents a case as “Total Knee,” another as “TKA.” Your reporting tool treats them as different procedures. Now your numbers are off before you even start analyzing.
Lagging Reports: In many departments, performance reports are generated monthly or quarterly. If a department chair gets a report showing how well the OR blocks were utilized for Q2, 45 days after the quarter is over, it’s useless. The behavior that led to low utilization is ancient history, and the chance to course correct has long passed.
Inconsistent Metrics: Trust is easily eroded in data analytics. If the finance team calculates “margin” = reimbursement- direct cost, but the surgical director calculates it differently, they are effectively speaking different languages. This inconsistency leads to countless meetings arguing about whose numbers are correct instead of discussing what the numbers represent.




Comments
Post a Comment